Tips for birth partners
 Supporting your partner during labour and birth can be a rewarding and bonding experience for both of you. Use the Personalised Birth Preferences plan in the app to help you think about both of your needs and choices for labour and birth.
Staying well-hydrated and nourished during the labour will help you to stay alert, so come prepared with non-perishable snacks and drinks. It is also okay to take a break occasionally, especially if labour is long. Chat about this with your partner before labour so everyone’s expectations can be met.
If you have helped to pack the hospital bag, you will know where to find a hat and nappy for your newborn baby, as these are the first things the midwife will ask you for.
Depending on hospital policy it may be possible to have more than one birth partner during labour. It is wise to check with your midwife ahead of time.
Supporting your partner during labour and birth can be a rewarding and bonding experience for both of you. Use the Personalised Birth Preferences plan in the app to help you think about both of your needs and choices for labour and birth.
Staying well-hydrated and nourished during the labour will help you to stay alert, so come prepared with non-perishable snacks and drinks. It is also okay to take a break occasionally, especially if labour is long. Chat about this with your partner before labour so everyone’s expectations can be met.
If you have helped to pack the hospital bag, you will know where to find a hat and nappy for your newborn baby, as these are the first things the midwife will ask you for.
Depending on hospital policy it may be possible to have more than one birth partner during labour. It is wise to check with your midwife ahead of time.
Tips for your birth partner
Ten tips for birth partners
 Sometimes babies are born so early or so unwell it is very hard for them to survive despite having intensive care. This will be a very difficult time for you and your family. Your baby will have fought so hard to have met you and spend time with you since their birth.
Whilst your baby is still alive, you may wish to make memories with them such as making prints of their hands and feet, taking photos and videos of you all together, introducing them to siblings and family they may not have met yet, reading them your favourite books and having a ceremony to celebrate their life. The neonatal team helping you to care for your baby will be able to assist you with all these things and any other requests you may have.
Sometimes babies are born so early or so unwell it is very hard for them to survive despite having intensive care. This will be a very difficult time for you and your family. Your baby will have fought so hard to have met you and spend time with you since their birth.
Whilst your baby is still alive, you may wish to make memories with them such as making prints of their hands and feet, taking photos and videos of you all together, introducing them to siblings and family they may not have met yet, reading them your favourite books and having a ceremony to celebrate their life. The neonatal team helping you to care for your baby will be able to assist you with all these things and any other requests you may have.
 Having a premature baby is the beginning of a long and emotional journey towards going home. It can be a very stressful time for your whole family. A premature baby’s development happens in the same order as it would have happened in your womb. When your baby reaches certain health, growth and development milestones, you’ll be able to take them.
All babies are different, and their behaviour and development are different too. In premature babies, the differences have to do with how premature they were when they were born.
Below are some changes that you can expect and watch out for in your premature baby and what you can do to help their development.
Having a premature baby is the beginning of a long and emotional journey towards going home. It can be a very stressful time for your whole family. A premature baby’s development happens in the same order as it would have happened in your womb. When your baby reaches certain health, growth and development milestones, you’ll be able to take them.
All babies are different, and their behaviour and development are different too. In premature babies, the differences have to do with how premature they were when they were born.
Below are some changes that you can expect and watch out for in your premature baby and what you can do to help their development.
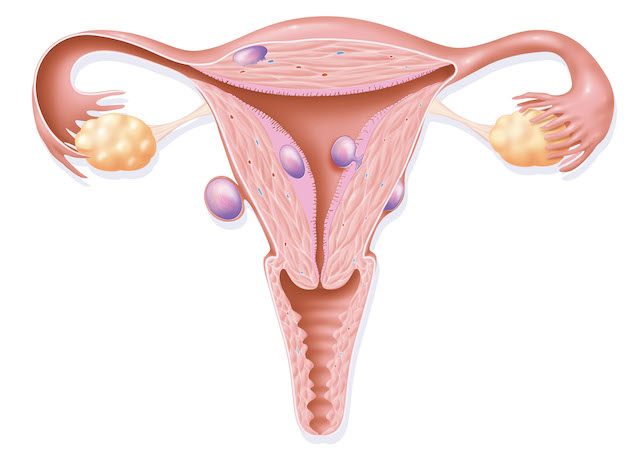
 Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
If your baby is too unwell to survive
If your baby is too unwell to survive
 Sometimes babies are born so early or so unwell it is very hard for them to survive despite having intensive care. This will be a very difficult time for you and your family. Your baby will have fought so hard to have met you and spend time with you since their birth.
Whilst your baby is still alive, you may wish to make memories with them such as making prints of their hands and feet, taking photos and videos of you all together, introducing them to siblings and family they may not have met yet, reading them your favourite books and having a ceremony to celebrate their life. The neonatal team helping you to care for your baby will be able to assist you with all these things and any other requests you may have.
Sometimes babies are born so early or so unwell it is very hard for them to survive despite having intensive care. This will be a very difficult time for you and your family. Your baby will have fought so hard to have met you and spend time with you since their birth.
Whilst your baby is still alive, you may wish to make memories with them such as making prints of their hands and feet, taking photos and videos of you all together, introducing them to siblings and family they may not have met yet, reading them your favourite books and having a ceremony to celebrate their life. The neonatal team helping you to care for your baby will be able to assist you with all these things and any other requests you may have.
End of life care for your baby
If the neonatal team has spoken to you about your baby dying, they may start to change the focus of their care from active care to focusing more on maximising their comfort. This may involve doing fewer painful procedures on your baby or starting your baby on some medicines to keep your baby comfortable. The team will discuss with you, whenever possible, about where you would like to be with your baby when they stop receiving active treatment and transition to receiving comfort-focused care. This is usually in hospital, but may be in a hospice, or even at home. The neonatal staff will support in making these decisions. The neonatal team may also introduce you to the palliative care team, who are experts in caring for babies with life-limiting conditions. The team will also discuss with you whether you would like your baby to have a postmortem examination to find out more about the problems that have made your baby so ill. There are also some instances where the coroner may make this decision.After your baby has died on a neonatal ward
The neonatal unit staff will support you to be able to provide care for your baby around the time of death. They will issue you with a death certificate and provide you with all the information you need about registering your baby’s death. You will be offered a bereavement appointment to talk about your baby’s care a few weeks after their death. A bereavement nurse will be in regular contact with you too.Helping your premature baby to develop
Helping your premature baby to develop
 Having a premature baby is the beginning of a long and emotional journey towards going home. It can be a very stressful time for your whole family. A premature baby’s development happens in the same order as it would have happened in your womb. When your baby reaches certain health, growth and development milestones, you’ll be able to take them.
All babies are different, and their behaviour and development are different too. In premature babies, the differences have to do with how premature they were when they were born.
Below are some changes that you can expect and watch out for in your premature baby and what you can do to help their development.
Having a premature baby is the beginning of a long and emotional journey towards going home. It can be a very stressful time for your whole family. A premature baby’s development happens in the same order as it would have happened in your womb. When your baby reaches certain health, growth and development milestones, you’ll be able to take them.
All babies are different, and their behaviour and development are different too. In premature babies, the differences have to do with how premature they were when they were born.
Below are some changes that you can expect and watch out for in your premature baby and what you can do to help their development.
|
23 to 27 weeks gestation |
|
| Weeks of gestation/Cues | What you can do to help |
|---|---|
| 23 weeks: Eyes are closed. Little movement. | Ask your baby’s nurse to show you how you can touch your baby. Familiarise yourself with the BLISS family handbook. |
| 24 weeks: Your baby’s skin is very thin and transparent. | Talk quietly to your baby as they can hear you. |
| 25 weeks: Your baby’s body is lean with no fat. His/hers arms and legs are limp. Your baby doesn’t yet have good muscle tone. | Ask your baby’s nurse about how to hold and position your baby. Leave a small piece of cloth that smells of you with your baby. |
| 26 weeks: Your baby’s eyes will start to open but they can’t focus yet. Your baby will sleep a lot. The breath triggering part of your baby’s brain hasn’t fully developed yet, so pauses between breaths are common. | Keep the lights as dim as possible. Shield your baby’s eyes from bright light to enable your baby to try and open their eyes. |
| 27 weeks: Your baby may startle at loud noises. | Avoid sudden noises. Remember positioning. |
|
28 to 32 weeks gestation |
|
| Weeks of gestation/Cues | What you can do to help |
|---|---|
| 28 weeks: Your baby’s movements may be jerky and jittery. Their hand grasp and sucking reflexes appear but these will be weak. | Ask the nurse about skin to skin contact (kangaroo mother care). Let your baby gently hold your finger. Your baby may take a non-nutritive tool. |
| 29 weeks: The ability to hear and smell will allow your baby to recognise you. | Talk softly to your baby when you visit. You may like to read short stories, nursery rhymes or sing to your baby. |
| 30 weeks: Your baby has periods of alertness and sleep Your baby may recognise your face now. | Try to observe the periods of alertness in your baby, to allow them to look at you and interact |
| 31 weeks: Your baby may be able to keep his/hers eyes open wide for a time. | Move your face back and forth slowly and your baby may follow you and your eyes. |
| 32 weeks: Your baby will be more interested in sucking and may appear to suck the feeding tube. | Offer a non-nutritive feed with tube feeds. Speak to your baby’s nurse about cup feeds if appropriate. |
|
33 to 37 weeks gestation |
|
| Weeks of gestation/Cues | What you can do to help |
|---|---|
| 33 weeks: There are clear sleep and awake cycles. Your baby will be moving around in the cot and incubator a lot. | Provide a calm environment around feeding time to enable your baby to focus on sucking, swallowing and breathing. |
| 34 weeks: Your baby may be sucking on hands and non-nutritive tools. | Offer the breast, or start using your own bottles and teats. Hold your baby still rather than rocking them to enable them to gradually become accustomed to position changes. |
| 35 weeks: Your baby may wake up when hungry, may cry with a wet or dirty nappy. | Allow your baby to gaze at your face. Talk or sing in a soft voice whilst your baby is in light sleep. |
| 36 weeks: Your baby may have a more consistent sleep/wake cycle. Your baby may want to be held and cuddled more. | Parents’ voices, smells and faces are very important. |
| 37 weeks: Your baby should be gaining more weight and has fuller cheeks. | Spend as much time as you can with your baby. If you haven’t talked about or arranged an overnight stay, this is a good time to book it. Ask the team about resuscitation training. |
37 weeks onwards
As long as your baby is well, now is the time to start building on what you and your baby have been doing from 35 weeks. Your baby should be gaining weight well, maintaining their temperature in an open cot and breast or bottle feeding.- Take short walks with your baby and try short periods of time with your baby in a bouncy chair.
- Use more interactive and visually stimulating toys.
- Talk to the neonatal team about structuring your baby’s day i.e. day/night/bath time/playtime.
- Make sure your home is ready for discharge.
- Make sure the baby’s Red Book (Personal Child Health Record Book) is completed before discharge from hospital.
Fibroids
Fibroids
 Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
Fibroids are benign (non-cancerous) growths that are found in or on the womb (uterus). Owing to their location they can have an impact on fertility and getting pregnant.
Uterine fibroids are relatively common. 30% of women between the ages of 25 and 44 have symptoms of fibroids. This means that uterine fibroids are common during a woman’s childbearing years. You may not even be aware that you have a fibroid until this shows up on an ultrasound scan.
Most women will experience no effects from fibroids during their pregnancy. Some women with fibroids will develop complications during pregnancy. Pain is the most commonly report complication, particularly if the fibroids are bigger than 5 cms.
Fibroids may increase the risk of other complications during pregnancy and birth. These include:
- Fetal growth restriction (slow growth) – large fibroids may prevent a baby from growing well as there is less space in the womb.
- Placental abruption – this occurs when the placenta comes away from the wall of the uterus because it is blocked by the fibroid.
- Preterm birth – pain from fibroids may lead to uterine contractions, which can result in the baby being born early.
- Miscarriage – the presence of fibroids increases the risk of spontaneous miscarriage in early pregnancy.
- Caesarean birth – the presence of fibroids increases the need for caesarean birth due to the location of the fibroids in the womb. If the fibroids are located in the lower part of the uterus, they may block the opening of the birth canal resulting in the need for caesarean birth.
- Postpartum haemorrhage – poor contracting can lead to bleeding after the birth. If the uterus is unable to contract because of the presence of fibroids, the blood vessels that supplied the placenta may continue to bleed. Postpartum haemorrhage (bleeding) is a medical emergency and usually occurs 24-48 hours after birth. You should get help urgently.
Miscarriage and the loss of your baby: Frequently asked questions
Miscarriage and the loss of your baby: Frequently asked questions
I have been told I have an early miscarriage, what support can I get?
A miscarriage affects every woman and her partner differently. It can be a very distressing time and you may experience a range of emotions: a great sense of sadness, anger, guilt, loss and grief after the event. It is important to ensure that you get the emotional support you need to recover. This can be simply talking to family and friends, particularly someone who has also experienced a miscarriage. If you feel you are struggling to cope you should also speak to your GP for advice and support.Why has this happened to me?
Unfortunately, early miscarriages,(pregnancies lost within the first 12 weeks i.e. first trimester) are very common, 1 in 5 pregnancies. It is not always clear why a miscarriage has happened although the majority of these are thought to be due to abnormalities in the chromosomes (genetic material or DNA) that make up the pregnancy. These are usually random abnormalities that occur at conception meaning the baby is unable to develop normally. A poorly formed placenta can also cause problems. All these problems are unlikely to occur again, and the most likely outcome is that your next pregnancy will survive to birth. There are certain factors that increase the risk of miscarriage that you cannot control, such as getting older. However, medical conditions such as uncontrolled diabetes or thyroid disease, as well as lifestyle factors such as smoking, caffeine intake and your Body Mass Index (BMI) can also increase the risk. These factors can be controlled and it is worth seeing your GP for advice to optimise your chances of a healthy pregnancy in future.What happens next and what are my management choices?
In some miscarriages, the body recognises that the pregnancy has stopped developing and you start to bleed, which is often associated with tummy pain. For some women there are no symptoms and the diagnosis is only made during a routine ultrasound scan. Your choice of treatment option is guided by the type of miscarriage you have and the advice from your specialist on your personal circumstances.- If you miscarry early, the pregnancy may naturally and completely come away from the womb, so you have a “complete miscarriage”. This type of miscarriage does not need any treatment.
- An “incomplete miscarriage” is where a miscarriage has started but not all the pregnancy comes away, leaving some pregnancy tissue in the womb.
- A “missed (delayed) miscarriage” is where the baby has died in the womb and the mother often has no symptoms such as pain or bleeding.
- If you have an “incomplete”, “complete” or “missed (delayed) miscarriage” there are potentially up to 3 different management options available. These are:
- expectant (watching and waiting for the pregnancy to pass naturally)
- medical, or
- surgical management.