Deep vein thrombosis in pregnancy
Deep vein thrombosis in pregnancy
 Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
Being pregnant increases your risk of developing deep vein thrombosis (DVT), with the highest risk being after you have had your baby. However, a DVT can occur at any time during your pregnancy, including the first three months of pregnancy.
Signs/symptoms
- Pain/tenderness in the leg behind the knee or in the calf.
- Feeling of heat in the affected area or a red discolouration of the skin.
- Swelling of the affected area.
- A pulmonary embolism may cause shortness of breath and chest pain, which comes on suddenly and worsens with deep breaths, coughing or chest movement.
Treatment
These conditions are serious and will require urgent treatment in hospital with medications that prevent the clot from getting bigger and breaking off and travelling to another part of the body.Prevention
- Keep mobile and rotate your ankles regularly.
- Wear compression stockings if your midwife or doctor have advised you to do so.
- Consider taking short walks when you feel up to it.
- Stay well hydrated.
- Avoid sitting/lying down for prolonged periods, ie, in a car/on a train.
Spontaneous Coronary Artery Dissection (SCAD) in pregnancy
Spontaneous Coronary Artery Dissection (SCAD) in pregnancy
 SCAD is a rare but serious heart condition that causes a tear or bruise to develop in a coronary (heart) artery resulting in a blockage that prevents normal blood flow. It can cause heart attack, heart failure or cardiac arrest and can be fatal.
SCAD can happen during pregnancy and during the weeks and months after you have given birth. Symptoms can include:
SCAD is a rare but serious heart condition that causes a tear or bruise to develop in a coronary (heart) artery resulting in a blockage that prevents normal blood flow. It can cause heart attack, heart failure or cardiac arrest and can be fatal.
SCAD can happen during pregnancy and during the weeks and months after you have given birth. Symptoms can include:
- central chest pain
- arm pain or numbness
- pain in the jaw, back or shoulders
- nausea
- sweating/clamminess
- breathing difficulties
Placenta accreta
Placenta accreta
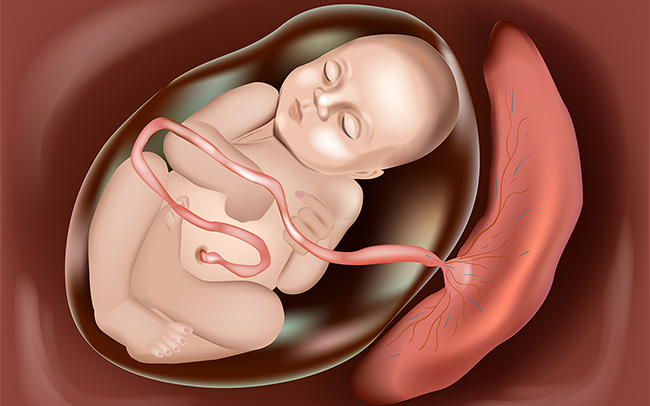 The placenta can also sometimes implant abnormally into the wall of the womb. This is a rare condition known as placenta accreta. The risk of having placenta accreta is higher if there is a previous scar on the womb, such as from a previous caesarean section, as the placenta can invade into the previous scar. This is a very serious condition that can be challenging to manage and a hysterectomy (operation to remove the womb) is sometimes needed at the time of delivery.
The placenta can also sometimes implant abnormally into the wall of the womb. This is a rare condition known as placenta accreta. The risk of having placenta accreta is higher if there is a previous scar on the womb, such as from a previous caesarean section, as the placenta can invade into the previous scar. This is a very serious condition that can be challenging to manage and a hysterectomy (operation to remove the womb) is sometimes needed at the time of delivery.
Placenta praevia
Placenta praevia
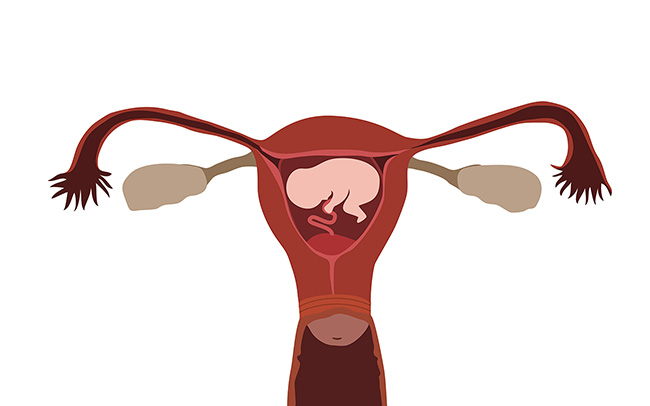 This can be picked up on an ultrasound scan as a low lying placenta in mid pregnancy. This is when the placenta is covering all or part of the entrance to the womb.
If you are found to have a low lying placenta you will be rescanned between 32-36 weeks. The majority of low lying placentas will move to the upper part of the womb by 36 weeks, however 10% of low lying placentas remain low. This can cause bleeding in pregnancy that is sudden and severe. A caesarean birth may be recommended in cases of severe placenta praevia, and the likelihood of needing a blood transfusion can be higher.
This can be picked up on an ultrasound scan as a low lying placenta in mid pregnancy. This is when the placenta is covering all or part of the entrance to the womb.
If you are found to have a low lying placenta you will be rescanned between 32-36 weeks. The majority of low lying placentas will move to the upper part of the womb by 36 weeks, however 10% of low lying placentas remain low. This can cause bleeding in pregnancy that is sudden and severe. A caesarean birth may be recommended in cases of severe placenta praevia, and the likelihood of needing a blood transfusion can be higher.
Intrahepatic cholestasis of pregnancy (obstetric cholestasis)
Intrahepatic cholestasis of pregnancy (obstetric cholestasis)
 This is a liver disorder that can develop in pregnancy, usually after 30 weeks gestation, but which sometimes develop as early as 8 weeks, affecting up to one in every 140 pregnant women.
Symptoms can include:
This is a liver disorder that can develop in pregnancy, usually after 30 weeks gestation, but which sometimes develop as early as 8 weeks, affecting up to one in every 140 pregnant women.
Symptoms can include:
- itching, usually on the hands and feet but which can be anywhere on the body
- dark urine, pale stools
- yellowing of the skin and whites of the eyes.
Pre-eclampsia (PET) during pregnancy
Pre-eclampsia (PET) during pregnancy
 This is a rare but serious condition of pregnancy, usually occurring after 20 weeks. It is defined by the combination of raised blood pressure and protein in the urine. Often there are no symptoms and pre-eclampsia is usually detected through regular antenatal checks, and can sometimes develop quickly.
Symptoms include:
This is a rare but serious condition of pregnancy, usually occurring after 20 weeks. It is defined by the combination of raised blood pressure and protein in the urine. Often there are no symptoms and pre-eclampsia is usually detected through regular antenatal checks, and can sometimes develop quickly.
Symptoms include:
- severe headaches
- sudden increase in swelling – particularly in the face, hands, feet or ankles
- problems with your vision such as blurring or bright spots before your eyes
- severe pain just below your ribs
- feeling very unwell.
Gestational diabetes
Gestational diabetes
 Gestational diabetes is high blood sugar that develops during pregnancy and usually disappears after the birth. It occurs when the body cannot produce enough insulin (a hormone responsible for controlling blood sugar levels) to meet the increased demands of pregnancy. Symptoms aren’t common, but many women are screened for this condition during pregnancy, particularly if they have certain risk factors. Ask your midwife if you are at risk of developing gestational diabetes and if you need to be tested.
Gestational diabetes is high blood sugar that develops during pregnancy and usually disappears after the birth. It occurs when the body cannot produce enough insulin (a hormone responsible for controlling blood sugar levels) to meet the increased demands of pregnancy. Symptoms aren’t common, but many women are screened for this condition during pregnancy, particularly if they have certain risk factors. Ask your midwife if you are at risk of developing gestational diabetes and if you need to be tested.
Gestational Diabetes Part 1
Gestational Diabetes Part 2
Gestational Diabetes Part 3
Less common pregnancy complications
Less common pregnancy complications
 If you have any symptoms of gestational diabetes, pre-eclampsia or intrahepatic cholestasis of pregnancy call your maternity triage/assessment unit straight away.
If you have any symptoms of gestational diabetes, pre-eclampsia or intrahepatic cholestasis of pregnancy call your maternity triage/assessment unit straight away.

